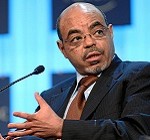
The untimely death of Meles Zenawi, the Prime Minister of Ethiopia, in a hospital in Brussels on 20 August 2012, once again highlights the condition of the healthcare sector in Africa.
So far in 2012, three other heads of state who were medically treated abroad, have died – Malam Bacai Sanha of Guinea Bissau was treated in France, Bingu wa Mutharika of Malawi was in hospital in South Africa, and John Atta Mills of Ghana went to the U.S. for treatment. [1] Since 2002, at least 10 heads of state of African countries have died after returning home or while in a hospital abroad.
In 2010, the Nigerian President Alhai Umaru Musa Yar’ Adua’s long absence for treatment in Saudi Arabia for a heart ailment made headlines across the continent. In May 2008, Robert Mugabe, the President of Zimbabwe, is reported to have undergone tests for cancer in Singapore. In 2007, the Egyptian President Hosni Mubarak had a successful gall bladder surgery in Germany.
This is not an exhaustive list; it only illustrates the fact that the leaders of Africa, the political elite, do not have faith in the medical systems of their own countries. They vote with their feet at times of medical emergencies and access healthcare beyond their own state borders.
Travelling overseas for healthcare facilities is not a new process, but it is becoming more common in many parts of the world. The trend of an international trade in health services was noted by the Organisation for Economic Cooperation and Development (OECD) more than two decades ago, in 1989. [2]
The privileged few in Africa who have big budgets, usually go to Europe for treatment. India is the destination for many from the middle and low income strata – they come here for high quality healthcare at relatively affordable prices in private hospitals. (Ironically, India spends only 4.2% of its GDP on health, well below several countries in Africa, and healthcare in our state-of-the-art private hospitals is unaffordable for the majority of Indians).
Large segments of the populations in African countries, who live below social safety nets and need effective healthcare, cannot afford expensive treatment in Europe, India, or elsewhere. They cannot even afford good medical treatment – if and when it is available – in their own countries.
What does a context of such disparity, where healthcare at home is inadequate or unaffordable, and only a few with the resources can travel overseas for treatment, say about the health sector in Africa? Why are medical facilities so inaccessible in so many parts of Africa?
Several factors contribute to the deficiency in healthcare in Africa. The public healthcare system in most parts of Africa is debilitated. With low investments in the health sector, hospitals are understaffed, and medical training colleges are inadequate. Low salaries and limited career prospects often compel trained medical professionals to migrate to other countries. Africa has 10% of the world’s population but 25% percent of the global incidence of diseases, and only 3% of the global health force. There are only two physicians per 10,000 persons in Africa, as compared to 32 per 10,000 in Europe. [3]
The healthcare sector in Africa is under-financed; many African countries are not committed to the Abuja Declaration of 2001, with which member states pledged to allocate at least 15% of their annual budget to the health sector. The total expenditure on health as a percentage of the GDP (2008) is between 4 to 6 % in Ethiopia, Kenya, and Nigeria, and 7 to 9 % in Ghana, Malawi, Rwanda, South Africa and Uganda. Only a few countries in Africa spend more on healthcare – around 13% of the GDP in Burundi, Liberia and Sierra Leone. [4] No country has reached the Abuja target, despite an overall increase in development assistance to health from donors. The funds are diverted to other budget heads by the national governments.
A regular supply chain of affordable medicines and pharmaceuticals is also not in place because of limited indigenous production of drugs and scarce medical research facilities. Weak regulation has meant that counterfeit drugs are easily available. Locally-produced drugs are often sub-standard. Expensive drugs have to be imported, which further increases the costs of healthcare.
The medical infrastructure in the private sector is relatively better in some countries such as South Africa, Mauritius, and Botswana, than in others. But private hospitals are expensive and beyond the reach of a majority of the people.
It is clear that the healthcare sector in Africa needs to be urgently reformed.
Long-term changes could be brought about by increasing the funding for healthcare, prioritising medical research in budget allocations, and by increasing the remuneration for health sector workers.
As an intermediate step, advanced medical care could be made available through public-private partnerships in hospitals. This is already being done in a few places – for example, at the private hospitals run by the Aga Khan Foundation in Kenya and Tanzania. These hospitals are unaffordable for the majority in Africa, but with the advantage of proximity they could be an option for treatment or follow-up within Africa for the middle class and for people who can pool in resources through family or social networks such as the Church.
To lower the cost of treatment, the governments of African countries could subsidise these partnership hospitals. A more viable alternative would be to build public hospitals that can hire the services of medical professionals from the private sector or from the general pool of medical professionals trained in the country, by offering them attractive salaries.
Policy-makers in Africa also need to address the contentious issue of the availability of affordable generic drugs, and reduce the continent’s dependence on exorbitantly-priced patented drugs made by multinational companies. They should not support anti-generic drug laws, as Kenya did in 2009. Inexpensive generic drugs for the treatment of HIV, supplied by a few Indian pharmaceutical firms, have made a big difference in Africa.
None of these changes are possible without transparent allocation of funds and good governance. The most significant reason for the poor state of healthcare in Africa is a lack of political will to overhaul the healthcare system. The political elite have access to foreign hospitals, and their bills are reimbursed by the state exchequers. [5] They don’t have to suffer the consequences of poor medical facilities in their own countries.
If it becomes mandatory for the political leaders of African nations to undergo medical treatment at home, or becomes difficult for them, through restrictive legislation, to pursue treatment abroad, the healthcare sector in Africa would probably improve rapidly. In Nigeria, the federal government is already planning to stop funding the foreign medical treatment of its leaders. With this, Nigeria could be taking a step to meet its commitment to the Abuja Declaration.
Civil society could also collectively oppose politicians who access medical treatment outside their own country. The combined legal and social pressure might force the governments to upgrade medical services at all levels, and this could eventually make healthcare available to all in Africa.
Renu Modi is the Africa Studies Fellow at Gateway House: Indian Council on Global Relations. She is the former Director of the Centre for African Studies, University of Mumbai.
This article was exclusively written for Gateway House: Indian Council on Global Relations. You can read more exclusive content here.
For interview requests with the author, or for permission to republish, please contact outreach@gatewayhouse.in.
© Copyright 2012 Gateway House: Indian Council on Global Relations. All rights reserved. Any unauthorized copying or reproduction is strictly prohibited.
1. Taylor Ian, 22 August 2012, ‘Why African presidents die abroad, SAFPI
, http://www.safpi.org/news/article/2012/ian-taylor-why-african-presidents-die-abroad.
2. OECD, 1989, Trade in Services in Developing Countries, Paris
3. WHO, 2009, ‘Health workforce, Infrastructure, Essential medicines, at <http://www.int/whosis/whostat/EN_WHS09_Tables6.pdf.
4. WHO ( 2011), ‘Health expenditure’ at http://www.who.int/whosis/whostat/EN_WHS2011_Full.pdf
5. Modi, R, 2011, ‘Healthcare of Africans in India’ in South- South Cooperation: Africa on the Centre Stage, Palgrave Macmillan, UK.